

On examination, he had difficulty with tandem gait, saccadic pursuit, extensor plantars, brisk upper limb tendon reflexes, reduced knee jerks, absent Achilles reflexes, mild peripheral atrophy in upper and lower limbs, reduced vibration sense peripherally in the lower limbs, pes cavus, and hammer toes. Following a further relapse with vertigo and gait unsteadiness, combined with MRI evidence of disease activity, he was switched to natalizumab and has remained relapse-free since. The episode was treated successfully with corticosteroids. Spinal cord MRI revealed a cervical T2 lesion compatible with demyelination (Figure 1(d)). Two years later, he had an episode of numbness affecting the extremities. He was then started on prophylactic treatment with beta-interferon. This remitted with corticosteroid treatment. Later that year, the patient developed gait unsteadiness, with further MRI evidence of disease activity.
The ON remitted following corticosteroid treatment but relapsed a few months later and was further treated successfully with steroids. CSF analysis revealed no oligoclonal bands (OCB) and normal IgG index. Visual evoked potentials were prolonged ipsilaterally. Brain MRI revealed multiple focal periventricular, callosal, and brainstem lesions, some gadolinium-enhancing, strongly suggestive of MS (Figures 1(a), 1(b), 1(c), and 1(e)). At age 46, he developed left-sided optic neuritis (ON). Nerve conduction studies confirmed the presence of a hereditary neuropathy with intermediate velocities. He reported pes cavus since childhood, but no other significant early symptoms. We present a case of a 52-year-old man diagnosed with MS five years previously, who had a family history of peripheral neuropathy with no male-to-male transmission. To date, there have been two reports of patients with CMTX that developed CNS demyelinating disease compatible with the diagnosis of multiple sclerosis (MS). Less commonly, clinical involvement ranging from extensor plantars to acute transient encephalopathy can be observed. Subclinical CNS involvement documented on brain MRI is not uncommon in patients with CMTX. X-linked Charcot-Marie-Tooth disease (CMTX) is a hereditary neuropathy caused by mutations in GJB1 coding for connexin-32 (Cx32), a gap-junction protein expressed in peripheral Schwann cells and oligodendrocytes within the central nervous system (CNS).
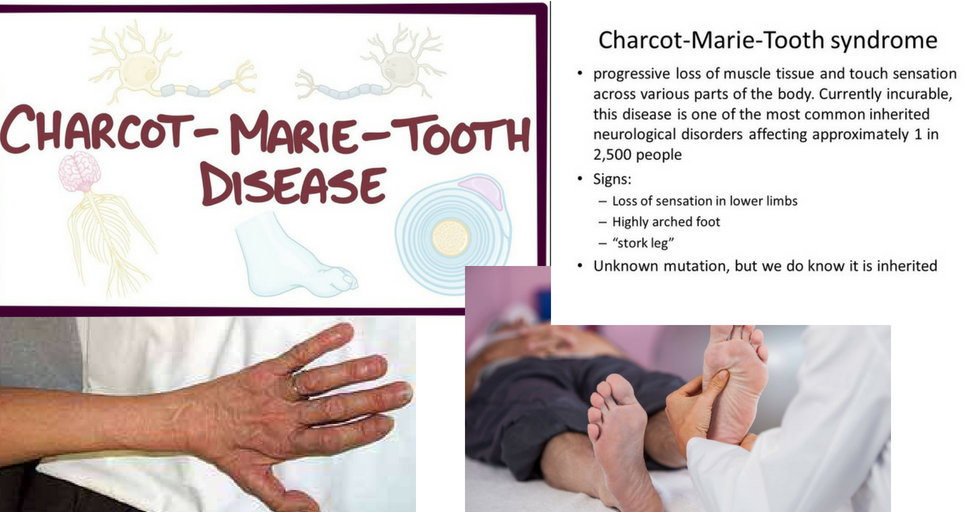
Although this may be a chance association, the increasing number of cases with CMTX and MS, especially with mutations involving the CNS, may imply some causative effect and provide insights into MS pathogenesis. This is the third case report of a patient with CMTX developing MS, but it is unique in the fact that other family members carrying the same mutation were found to have asymptomatic central nervous system (CNS) involvement (diffuse white matter hyperintensity on brain MRI and extensor plantars). Cys64Tyr) which was recently reported by our group. We report a patient with relapsing remitting multiple sclerosis (MS) and X-linked Charcot-Marie-Tooth disease (CMTX), carrying a GJB1 mutation affecting connexin-32 (c.191G>A, p.


 0 kommentar(er)
0 kommentar(er)
